TrendsFive key trends in the industry and practice emerged in the survey responses from community pharmacists, payers and technology vendors. The trends are reflective of healthcare in transition from fee-for-service and a volume-basis to pay-for-performance and a value-basis. The following trends are foundational to the recommended actions of this guide and offer additional context for those recommendations. 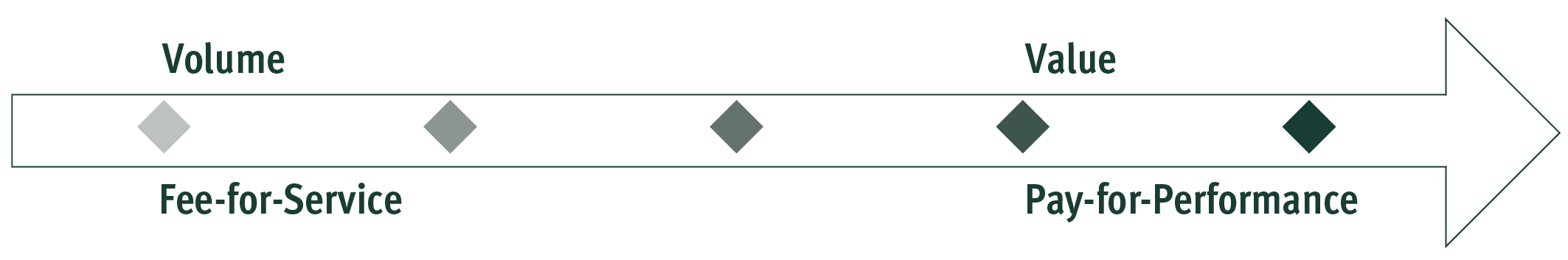
TransformationThe practice of community pharmacy is transforming from a foundation in product reimbursement and fee-for-service models, to pharmacy pay-for-performance and models in which quality and value are measured and incentivized. The transition to these emerging payment models includes incentives for improving health outcomes, enhancing patient experience and reducing the total cost of care for patients, payers, providers, and the healthcare system. Healthcare payers are changing their existing relationships with community pharmacy partners to develop clinical programming in chronic disease states such as hypertension, dyslipidemia, diabetes, asthma, mental and behavioral health, cardiovascular disease (e.g. congestive heart failure, coronary artery disease, stroke), and pain management and opioid use. OutcomesThe organization of value-based pharmacy networks and the use of pay-for-performance models for pharmacies has grown rapidly over the last five years in a market increasingly focused on value and outcomes. The ongoing transition of care and reimbursement to a value basis is shifting the focus of pharmacists and payers to outcomes and activities to achieve those outcomes. Pharmacists and payers have begun to collaborate in the identification of shared outcomes and development of clinical programming, value initiatives, and performance incentives. A focus on outcomes and the vertical integration of performance measure sets is predicted to support this alignment such that value extends into both the pharmacy benefit and the medical benefit through optimizing treatment outcomes. AlignmentPharmacists and payers are committing resources to improve care through a variety of strategies, including patient and pharmacist education; technology vendor partnerships; data analytics; enhanced services program development; and business intelligence support. The desired outcomes, goals, metrics, and incentives are often misaligned between pharmacists, payers, providers, and patients. As a result, business operations, financial, and clinical strategies within an organization are also misaligned with those external to the organization relating to managed care, health systems and community pharmacies. DataStandardization in data utilization, provider system interoperability and accessibility, management of the increasing volumes of data and limitations to the actionability of the information are only a few of the broad data challenges. Pharmacy organizations and payers encounter these challenges in the improvement of medication adherence, health outcomes, operational efficiencies and business results. Pharmacies are also burdened by the testing of scalability, predictability and measurability of new solutions prior to widespread implementation. Additionally, payers are encountering inefficiencies when having to creatively solve for individual integration issues. The channels to support the exchange, flow and integrity of data among pharmacists, payers, providers, and patients exist, but need to be further developed and before broader marketplace adoption can take place. CollaborationCollaborations between community pharmacists, healthcare payers, technology vendors and other stakeholders are becoming more critical in a market, industry and practice that continues to consolidate, vertically integrate and expand. The long-term viability and successful implementation of partnerships has become increasingly dependent upon the right people establishing trust and transparency, focusing on meaningful shared goals, establishing longitudinal relationships, sharing risk and coordinating successful implementations. Collaboration is the common element in the solutions and strategies to achieve the shared goals in value-based reimbursement arrangements and aligned clinical, humanistic and financial outcomes. Organizations acting as a neutral convener have emerged as a key element for success in early collaborations.
|
