|
actions to expand pharmacist-provided care 
Pharmacies and Payers TogetherPharmacists and payers together can consider taking five actions to develop and implement scalable pharmacist-provided care models. The perspectives of the pharmacists and payers participating in an industry survey and multi-stakeholder roundtable has been summarized in these recommendations. 
Identify clinical areas to expand the use and demonstrate the value of pharmacist-provided care.Pharmacists and payers should identify areas where patient-centered, pharmacist-provided care can be used more broadly to improve patient outcomes. From addressing medication and immunization gaps to managing chronic conditions or promoting smoking cessation, there are numerous clinical areas ripe for improvement initiatives that can demonstrate the value of pharmacist-provided care. In identifying and developing care programs, pharmacies and payers should establish: clear goals; program responsibilities; implementation requirements; and appropriate reporting, measurement, incentives and reimbursement. The programs developed and validated through pilot initiatives can inform the refinement of best practices, accreditation standards and clinical care guidelines.

Identify shared patient outcomes and goals for pharmacists and payersPharmacists and payers together should identify shared goals for patient outcomes. Shared goals will facilitate the development of specific care programs, clear metrics for evaluating care and appropriate incentives and reimbursement for care. Chronic disease management, for example, is a growing area of clinical need, where pharmacist-provided care can improve quality of life and reduce healthcare costs. Goals for patient populations should be similar across payers in order to support pharmacists in the standardization of patient engagement and care innovation for different segments of the populations. Pharmacists and payers can jointly determine which interventions are most valuable for the payer’s patient population and how use should be measured and compensated. See Figure 2 for prospective outcomes goals. Neutral organizations, such as multi-stakeholder quality organizations, can assist in the identification of shared outcomes by convening public and private payers, pharmacists and other stakeholders to achieve consensus. These organizations can also help resolve data reporting issues similar to those outlined below. Figure 2: Shared Outcomes and Goals of Pharmacists and Payers 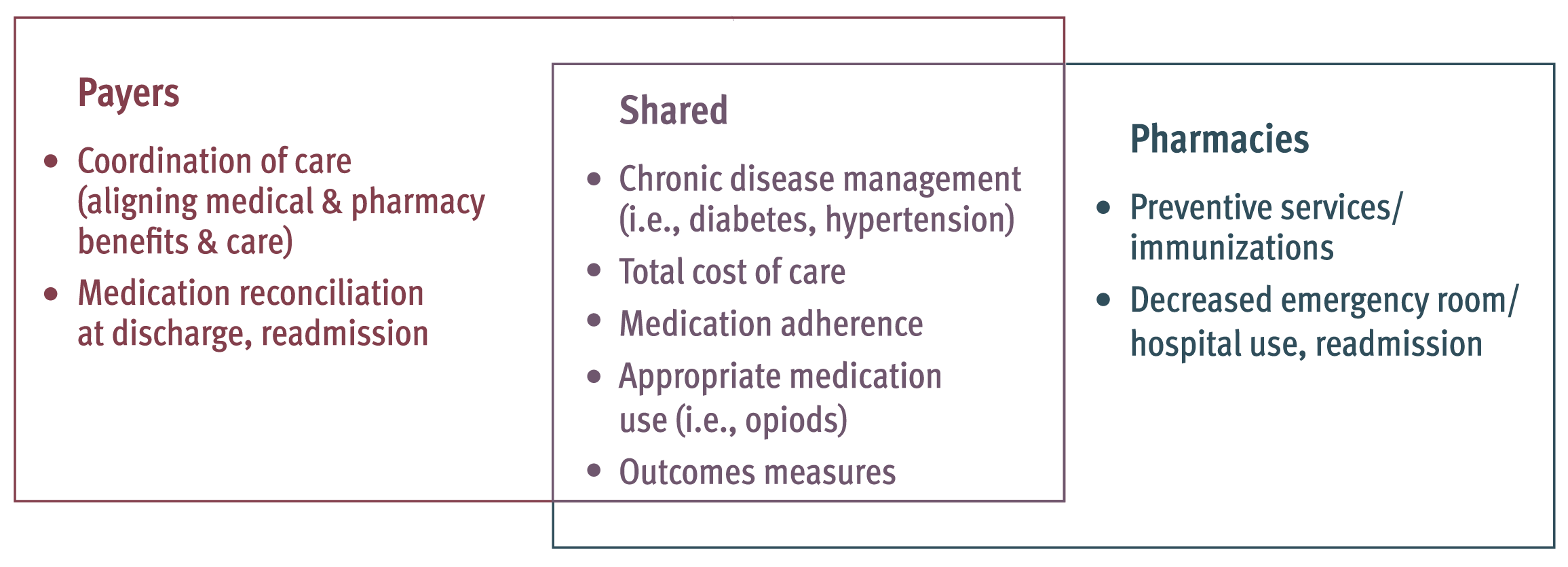
Source: Sync-to-Serve Survey Responses

Align strategies among pharmacists and payers to integrate the value of pharmacist-provided care.Clinical, operational and payment strategies need to be aligned among pharmacists and payers spanning Medicare, Medicaid and commercial plans. This alignment will allow pharmacist-provided care models to match the care requirements and goals of diverse payers. Vertical alignment also may address some of the legal, regulatory and contractual barriers that prevent the greater use of pharmacist-provided care. 
Implement pharmacist-provided care in all community pharmacies.With increasing emphasis throughout healthcare on patient outcomes and paying for value, pharmacist-provided care is a sustainable and effective model that moves beyond fee-for-service to value-based care. It should be implemented in all community pharmacies. Pharmacists and payers should begin by identifying the shared patient populations who would most benefit from pharmacist-provided care. Implementation should be expanded in unison with the payment for care to ensure the sustainability of clinical programs. Patient engagement in pharmacist-provided care offers pharmacists a way to provide useful, cost-effective care that meets the needs of payers and patients; especially high-risk patients with multiple chronic conditions taking multiple medications. Payers should coordinate the promotion of pharmacist-provided care with pharmacies to prevent patient confusion of available programs and further enable this patient engagement. The sharing of risk between pharmacists and payers is essential to support the delivery of pharmacist-provided care through pharmacies in socioeconomically challenged areas. 
Prioritize patients to receive pharmacist-provided care across all payers.High-risk and vulnerable patients benefit the most from pharmacist-provided care. To improve population health and lower overall healthcare spending, the highest-risk and most vulnerable patients should be prioritized for pharmacist-provided care, regardless of payer. Pharmacists and payers should collaborate to identify, prioritize, engage and care for these patients. Pharmacies and payers must improve information sharing to prioritize patients, establish reasonable performance expectations, and ensure appropriate pharmacy staffing and resources. By prioritizing patients based on their needs, pharmacist-provided care can support the best individual and population health outcomes, regardless of payer. Prioritizing and caring for high-risk patients in a multi-payer environment requires consideration of these issues, when establishing contract terms and benchmarks.
|
